The accounting firm’s latest financial performance survey – widely regarded as the best picture of the sector’s viability – shows the number of providers running at a loss has grown by 8% over the 12 months to June 2020 – even before the expenses from COVID are factored in.
The survey – which looked at data from 1,190 aged care homes representing 47% of the sector and 44,647 home care packages across Australia representing 33% of the sector – has excluded COVID-19 subsidies and expenses from its analysis to ensure the comparison of results with the previous year was “comparing apples with apples”.
Occupancy and profits down – but care hours up
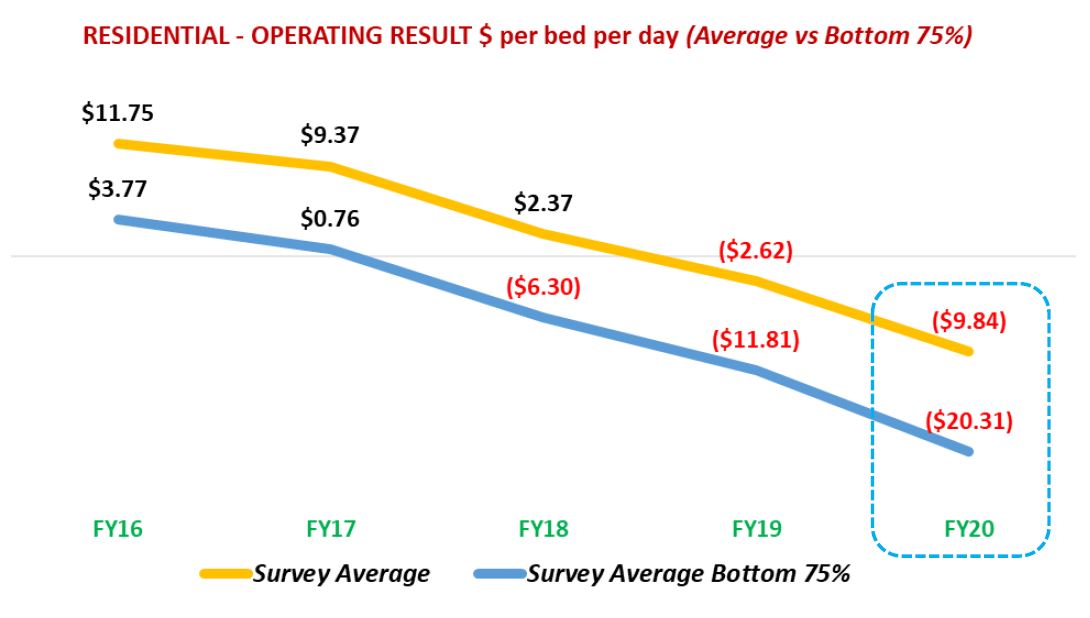 Almost two-thirds of aged care homes (64%) have recorded an operating loss for FY20 (compared to 56% for FY19), while 36% of aged care homes recorded an EBITDAR loss (operating cash loss) for FY20 (compared to 28% for FY19).
Almost two-thirds of aged care homes (64%) have recorded an operating loss for FY20 (compared to 56% for FY19), while 36% of aged care homes recorded an EBITDAR loss (operating cash loss) for FY20 (compared to 28% for FY19).
Occupancy levels for survey participants dropped to 91.4% average occupancy compared to FY19 when occupancy was 92.3%.
Average ACFI per bed day (pbd) did increase by $3.64 pbd to $181.42 pbd (or 2.05% pa), but direct care services costs also went up by $8.04 pbd to $156.99 pbd (5.4% pa).
Operators still managed to deliver increased care too, with total care hours per resident per day going up by 0.08 hours to 3.21 hours (FY19: 3.13 hours).
But overall, the average operating results for aged care homes fell significantly by $2,467 per bed per annum (pbpa) to a deficit of $3,371 pbpa in contrast to FY19 where the deficit was $904 pbpa.
Home care performance also fell marginally
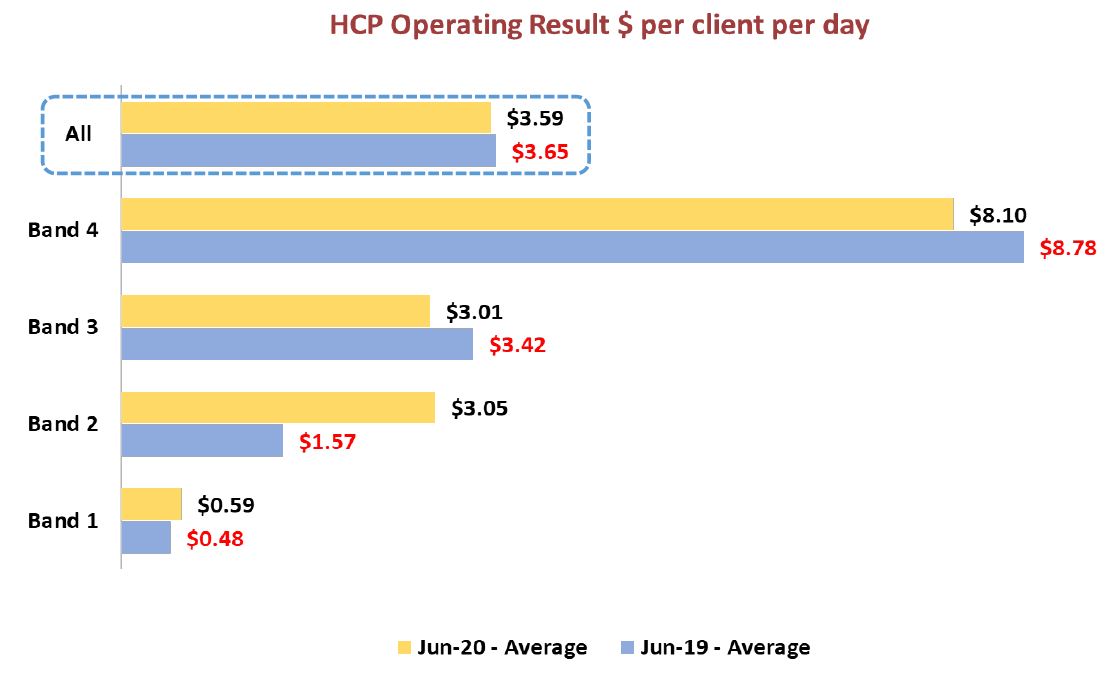 Home care performed only marginally better.
Home care performed only marginally better.
Revenue per client per day (pcpd) average dropped by 1.6% (being $1.15 pcpd) among the survey participants.
The average operating profit per client day marginally decreased by $0.05 pcpd to $3.59 pcpd, compared to $3.65 in FY19.
The average operating result also declined by $2.76 pcpd for the nine months from October 2019 to June 2020, while the average unspent funds per client increased by $1,846 per client (to average $8,841 per client).
Interestingly, given StewartBrown Senior Partner’s recent LASA presentation on home care hours, it was noted that staff hours per client per week have also declined by another 0.47 hours to an average of 5.63 hours per week.

Even the top 25% of home care providers fared worse, with the revenue per client per day (pcpd) average falling by 8.2% to $7.36 pcpd.
Conclusions – over 800 homes in trouble
StewartBrown concludes that the residential care sector has experienced a significant decline in its financial performance and sustainability – both before and after any COVID funding support.
They argue additional specific targeted funding and structural reform around accommodation revenue need to be implemented now to avoid further deterioration in the operating results and the potential increase in provider failures.
In particular, the report highlights the bottom 75% of aged care homes (835 homes) in the survey and their operating loss of $20.31 per resident per day.
“Given the number of homes this represents, this confirms that there is an urgent requirement for additional funding and a sustainable funding model going forward,” it states.
The analysis also notes the impact this would have on investment in the sector, including new builds, major refurbishments and improvements to existing homes.
Unspent funds a growing cause for concern
StewartBrown also points to a decline in home care operating results over the past nine months.
“Revenue per client day has reduced and, importantly, average staff hours per client have reduced to potentially unstainable levels,” it writes. “The mix between appropriate staffing and revenue will dictate the ongoing financial performance of the home care sector.”
Unspent funds are pinpointed as the biggest issue, now averaging $8,841 per client (care recipient) or over $1 billion in unutilised funds across the sector.
While the firm says the changes to payment arrangements to arrears instead of in advance will address this issue, the analysis concludes that this will have serious cash flow implications for providers that will need to be considered and monitored.
“Based on legislation introduced to the parliament to enact these changes, providers will have a choice of drawing down on the unspent funds rather than receive the subsidy so as to use them up and effectively transfer the unspent funds balance to the government or continue to hold and account for the unspent funds balances and return them to government and the care recipient at the end of their time as a home care consumer (in line with current procedures) until all unspent funds balances are utilised,” it says. “Providers can choose either method for each care recipient. The choice to opt-in to the drawdown method will occur during a six-month window from 1 September 2021.”
An important point for providers to consider.