You’d have to have your head buried in the sand not to see the growing crisis of ‘bed block’ across Australia’s hospitals.
This week’s headlines have been dominated by the standoff between the Federal Government and the States over who should pay for a health system that’s visibly buckling.
Case in point: NSW says one in five hospital beds are now occupied by someone waiting for an aged care placement – costing taxpayers $1.2 million a day.
Behind those figures is the real human toll. One patient spent 410 days waiting for an aged care bed – over 13 months lying in a hospital ward, losing strength, mobility and independence. This is no way to live.
A shortage of capability
The problem isn’t just space. It’s the lack of clinical capacity in the community to care for complex, medically fragile patients once they leave hospital.
Many of these so-called “bed blockers” are older adults with multiple conditions who’ve become deconditioned during long hospital stays. Others require higher clinical support – intravenous therapy, wound management, or 24/7 monitoring – that standard home care or aged care homes simply can’t deliver.
The blockage isn’t just a lack of beds; it’s a lack of options.
A reactive system, not a preventive one
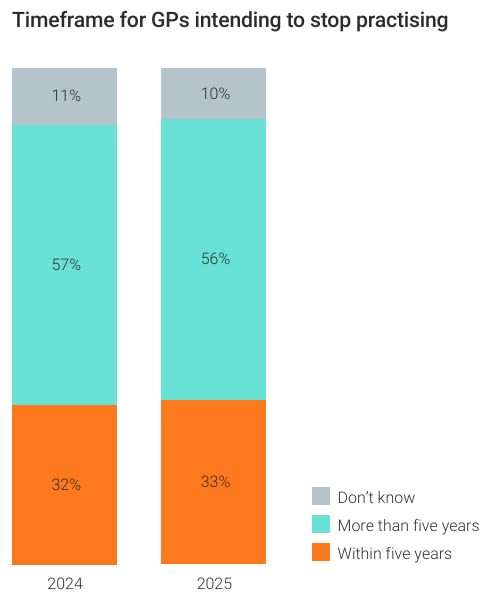
Since 2014-15, per-person hospital spending has jumped 30%, while funding for general practice has barely moved, according to the RACGP’s Health of the Nation 2025 report. One in three GPs now plans to quit within five years – see below.
We’re funnelling billions into acute care – while neglecting the front line that keeps people out of it.
The solutions aren’t mysterious. Yes, Australia needs more aged care beds and more Home Care Packages – but we also need to stop treating hospitals as the first and last resort.
That means a focus on prevention – and on alternative models like Hospital in the Home.
The real cure
During COVID-19, Hospital in the Home services flourished, proving that complex care could be safely delivered outside hospital walls. Yet Australia has fallen behind other nations. Providers say up to 10% of current hospital admissions could comfortably be managed at home – if funding allowed.
With less than three weeks until Support at Home begins on 1 November, it’s still unclear if patients discharged with clinical needs will be eligible for new funding for Short Term Restorative Care and palliative care if they don’t already hold a Home Care Package – leaving hospitals clogged and patients stuck.
Meanwhile, Queensland and South Australia are showing what’s possible. Both fund transitional “halfway house” programs through Hospital in the Home providers such as Amplar Health’s Pullman Hotel model in Adelaide, helping move hundreds of older patients out of hospitals and into supported settings.
Political blame-shifting won’t free the patients stuck in hospital – or keep Australia’s health system afloat. The cure isn’t more money, it’s more imagination.











