The final three days of the Sydney hearings saw ‘best practice’ providers, aged care staff, medical experts and dementia advisors all take a seat in the witness box – but it was Monash University’s Head of Health Law and Ageing Research Professor Joseph Ibrahim (pictured) who stole the show.
(The full daily reports are available in our newsletter The Daily COMMISSION. Subscribe HERE).
Professor Ibrahim – who is well-known for his research on preventing injuries in aged care – says his research shows nothing has changed in 15 years to reduce harm to residents, because there is no accountability in the system.
“They’re citizens of the State but the State doesn’t provide care because the Federal Government is supposed to. The Federal Government doesn’t provide care because the State is supposed to. Clinical care is the hospital run by the State, not by federal.
“GPs paid through the federal department, clinical care in the Act is the responsibility of the provider. Provider has no responsibility over the clinicians. The clinicians who provide the care have no obligation to the provider,” he stated bluntly.
Professor Ibrahim also lambasted the Department of Health for the lack of available data around injuries to aged care residents.
“We set up a system which is not accountable to anyone, so there has been no accounting by the Department of what they’ve done with that data for 10 years now and no one seems interested in that fact.”

This argument was backed up by evidence from witnesses from the Department, including the Chief Medical Officer Professor Brendan Murphy (pictured above) and Amy Laffan , the Assistant Secretary for the Aged Care Quality and Regulatory Reform Branch in the Department of Health.
Professor Murphy revealed the Department doesn’t have data on the prescribing of psychotropic drugs, benzodiazepines and antipsychotics or how many GP’s are prescribing then, but they are in the planning stages to gather this data publicly available.
“I think shining a light on this practice, probably at the facility level, subject to review by the Commission, it would be the best way to achieve it, and also to get national data,” he said.
Senior Counsel Assisting Peter Gray QC also grilled the Department of Health witnesses and the Aged Care Quality and Safety Commission (ACQSC)’s Executive Director, Christina Bolger (pictured below), on whether the new amendments to the Quality Principles around restrictive practices would be adequate.
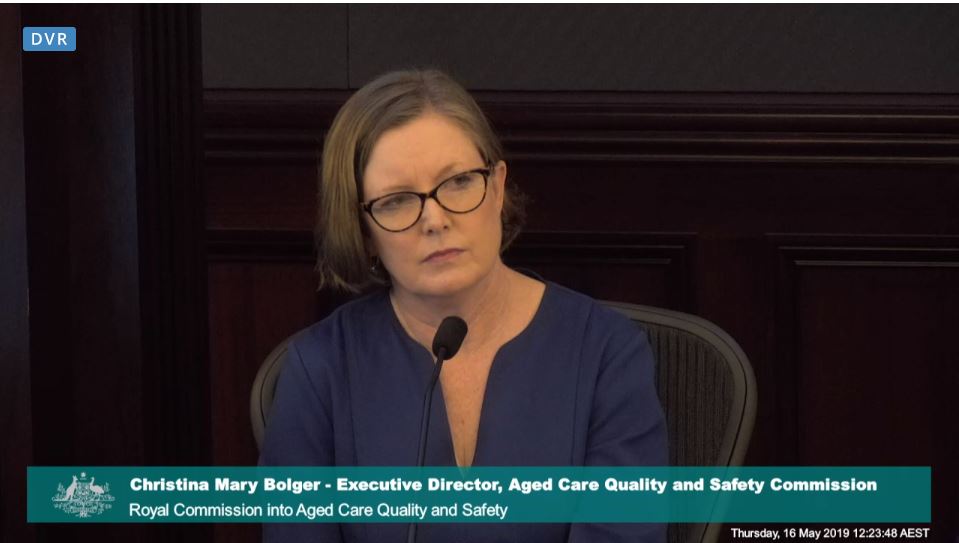
Ms Bolger conceded many of her recommendations did not make the final cut – and there was a potential gap in compliance monitoring for the new principles between 1 July (when they start) and 31 December 2019 (when the Commission begins its new regulatory role).
“It’s a matter, isn’t it, of the potential outcome indirectly being that a breach of new sections 15F and G [the new principles on restrictive practices] might be brought to the attention of the Commission and then the Commission would bring it to the attention of the Department, but the Commission isn’t setting out to monitor compliance with those sections?” Mr Gray asked.
“Technically no, but this is an area of high priority for the Commission, and it is supporting many of the outcomes under the aged care quality standards, so it’s not an area that will go unchecked,” Ms Bolger stated.
See below for Senior Counsel Assisting Peter Gray QC’s final points.